Asthma & Anaphylaxis Emergency in the Home

Allergy and Asthma
 If asthma or anaphylaxis are very real threats to you, a family member, or a friend, it is important that both you and your home are prepared.
In order to be ready for an asthma or anaphylaxis emergency you should follow 3 steps:
If asthma or anaphylaxis are very real threats to you, a family member, or a friend, it is important that both you and your home are prepared.
In order to be ready for an asthma or anaphylaxis emergency you should follow 3 steps:
- Reduce the risk of an emergency by removing triggers
- Know the symptoms so you can act quickly
- Know how to react in the event of an emergency
Reduce the Risk of Asthma and Anaphylaxis
The factors that cause someone to have an anaphylactic or asthmatic reaction are called ‘allergens’ or ‘triggers’. For someone with anaphylaxis or asthma, it's critical that trigger substances be removed from the immediate environment to reduce the risk of anaphylaxis or an asthma attack. In order to ‘trigger proof’ your home, you first need to know what the triggers are. Triggers vary from person to person. You'll need to know what would cause the individual in question to react adversely. You will need to ask the person if this is new territory for you. Anaphylaxis Triggers Anaphylaxis is a life-threatening allergic reaction. You are more likely to experience an anaphylactic attack if you have previously had an allergic reaction to something. Common allergens include foods such as:- Milk
- Eggs
- Peanuts
- Tree nuts
- Sesame
- Fish
- Shellfish
- Wheat
- Soy
- Bee
- Wasp
- Ant bites
- Over the counter
- Prescribed
- Herbal/alternative
- Cigarette smoke
- Exercise
- Inhaled allergens (e.g. pollens, moulds, animal dander, and dust mites)
- Environmental factors (e.g. dust, pollution, wood smoke, bush fires)
- Chemicals and strong smells (e.g. perfumes, cleaning products)
- Some foods and food preservatives, flavourings, and colourings (uncommon)
- Colds and flu
- Certain medications
- Emotional factors (e.g. laughter and stress)
- Changes in temperature and weather
Know the Symptoms of Asthma and Anaphylaxis
So you can act fast in an asthma or anaphylactic emergency in the home, the next step is to know the symptoms.Anaphylaxis symptoms include:
- Tightness of the throat from swelling
- Difficulty breathing
- Tongue and facial swelling
- Hoarse voice or difficulty speaking
- A wheeze or persistent cough
- Collapse or falling unconscious
- Becoming pale or floppy (young children)
- Abdominal pain and vomiting
- Hives, welts and body redness
The most common asthma symptoms include:
- Wheezing
- Shortness of breath
- Chest tightness
- Coughing fits
- Difficulty breathing
- Dry, irritating, persistent cough, particularly at night and early morning
- Gasping for breath, having little or no wheeze due to lack of air movement
- Severe difficulties breathing
- Severe chest tightness
- Only able to speak a few words at a time
- Feeling distressed and anxious
- Blue discolouration on or around the lips (if skin colour also changes this can be hard to see)
- Pale and sweaty skin
- Sucking in of throat and rib muscles
- Using shoulder muscles or bracing with arms to help with breathing
- Symptoms rapidly getting worse or frequently using reliever more than every 2 hours
- Children may become restless, unable to to settle or become drowsy
- Children may also have trouble eating and drinking due to shortness of breath
- A child may have severe coughing or vomiting

How to Respond to Asthma and Anaphylaxis
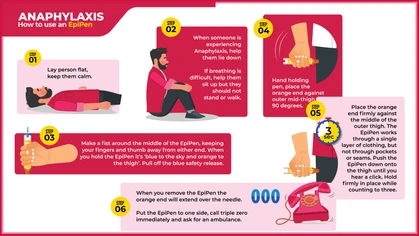
No matter how well you trigger proof your home, in sensitive cases, it takes just a small amount of the allergen to set off an attack. For that reason, make sure you know how to react to an anaphylaxis and asthma emergency in your home. First Aid for Anaphylaxis- Lay victim flat, do not stand or walk, or if laying down makes breathing difficult you should allow them to sit
- Prevent further exposure to the triggering agent if possible
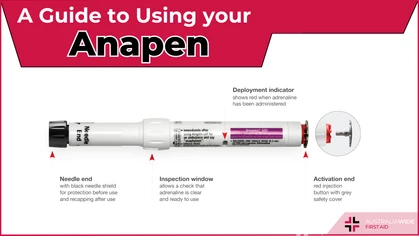
- Administer adrenaline through auto-injector such as an Epipen or Anapen
- Call an ambulance (even if they appear to be ‘getting better’)
- Further adrenaline should be given if no response after five minutes
- If breathing stops, commence CPR immediately
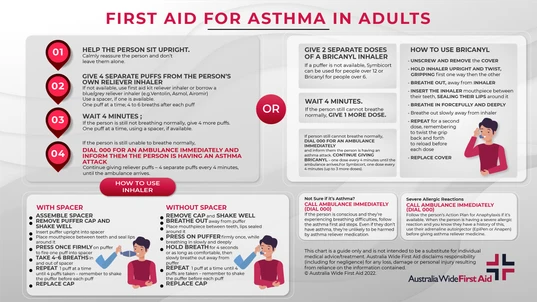
- Without delay give 4 separate puffs of a “reliever,” best given one puff at a time via a spacer device (if a spacer is not available, simply use the puffer).
- Ask the person to take 4 breaths from the spacer after each puff of medication.
- Use the person’s own inhaler if possible. If their own is not available or they don’t have one, use a first aid kit inhaler if available, or borrow one from someone else.
- Wait 4 minutes.
- If there is little or no improvement, give another 4 puffs as above.
- If there is still no improvement after the second round of treatment, call an ambulance immediately.
- Keep giving 4 puffs every 4 minutes until the ambulance arrives.
Learn Asthma First Aid
Asthma emergencies can be frightening, confusing, and even life-threatening. Arm yourself with the knowledge of how to recognise and treat an asthma episode and asthma emergency with our fully-online Asthma First Aid course. Or if you need asthma knowledge and skills for your workplace, our Workplace Asthma Management and First Aid gives you the skills and knowledge to be able to develop an asthma risk assessment and emergency management strategy to handle asthma episodes in the workplace. If you want to go one step further, our Workplace Asthma and Anaphylaxis Management and First Aid course also includes what you need to know about allergies and anaphylaxis. All of our online courses can be completed at your work desk or in the comfort of your own home, with a Certificate of Completion to hand to your employer, put on your resume, or simply give you the peace of mind knowing that you can actually be helpful in an emergency situation.
Originally published at
https://www.australiawidefirstaid.com.au/resources/ready-asthma-anaphylaxis-emergency-home
as part of the Australia Wide First Aid Articles Library